Interstructural Tissue Release and Integration
Lesson 4

Fascia
Fascia, also called connective tissue, surrounds as well as supports each muscle fiber, tendon, nerve, blood vessel and bone, so that they stay in place. It is made up of microscopic collagen fibers shaped into tiny tubular structures, a protein called elastin, to create flexibility and oily goo called hyaluronan so the collagen structures move freely over bones. It is also innervated with fibroblasts that communicate with each other, creating a neural network responsive to many types of trauma or behaviors. They can also contract the tissue as well as weave it like tiny spiders.
Adipose tissue is a specialized fascia consisting of lipid-rich cells called adipocytes. As it comprises about 20-25% of total body weight in healthy individuals, the main function of adipose tissue is to store energy in the form of lipids. Based on its location, fat tissue is divided into parietal (under the skin) and visceral (surrounding organs).
Loose connective tissue is a type of connective tissue with loosely arranged collagen fibers. However, it consists of many cells. Loose connective tissue is the most common type of connective tissue in vertebrates and it holds the organs in place and attaches the epithelial tissue to the underlying tissues. It mainly surrounds the blood vessels and nerves. Fibroblasts are widely dispersed in the loose connective tissue, secreting protein fibers and proteoglycans to the extracellular matrix.
Dense Connective Tissue: Dense connective tissue is a type of connective tissue that contains numerous collagen fibers and provides a strong connection between the tissues that mainly form the structural parts of the body.
Fascia responds to a sedentary lifestyle and poor posture by thickening near the joints, and becoming sticky. When it dries up and tightens around muscles, it can limit mobility, cause pain and bundle into mounds of this rubbery tissue. If you are active, this is less of a problem. However, if you experience a trauma or injury, the same bundling occurs to protect the joints.
80% of my work in clinic dealing with chronic pain origins in fascia bundling, This can affect posture, gait and alignment of hips, back or shoulders. This fascia is everywhere in your body! More than 20% of your body mass is fascia. Yet, most folks know very little about fascia. Carpenters know it as a flat material covering the ends of rafters, or molding as a superficial layer for decoration, to hide the joints and joists. This body fascia is also a covering, but it has critical functionality in the way we move. It is really a sensory organ that simultaneously observes and facilitates our movement and posture.
Fascia continuously transmits and receives mechanometabolic information that can influence the shape and function of the entire body. The fascia influences not only movements, but emotions as well. The presence of a disorder of the myofascial network during daily movement and activity can alter the emotional state of a person. The human being is a fascial being that walks. We are the living expression of bio-tensegrity as opposed to bio-mechanics
Biomechanics, by definition, is the study of mechanics and its relationship to the human body.
Biomechanics views the human body as a mechanical being. The truth is that our bodies aren’t robotic. We are not machines and cannot be diagnosed and repaired like a machine.
In Biomechanics, bones are the foundation of the human body. Bones and their joints take the load. As time passes this load bearing makes joints susceptible to conditions such as osteoarthritis.
Bio-tensegrity looks at this differently.
That difference between the biomechanics and bio-tensegrity is that in bio-tensegrity the muscles and facia around the bone distribute the weight, rather than the bones and joints.
This belief holds that, if you maintain your muscles to be strong and limber, as well as keep the Interstructural tissue pliable the tissue will absorb the load as a system rather than each individual bone.
As a Bodyworker, how can I help keep the fascia pliable and manage bundling?
Fingertips work from the affected joint out away from the heart. in small but firm motions, smooth out the bundles from the joint, If stubborn, use vibration for one minute, holding the tuning fork as close to the skin without touching it as possible. Repeat the process. Use Yin stretches after the tissue manipulation then gentle traction, and check if the bundling is smoothed out. Ask the client about pain, 1 to 10 where and with what motion it arises.
If there is still an issue, repeat the whole process again. What do you feel? Are you making progress? Is there tension in the tissue? If tension remains, check the associated chakra to make sure there's not a blockage. If there is, open it with vibration and then check the tension of the tissue. If the tension is reduced, then repeat the initial process one more time and the issue should be resolved.
If there is still an issue, look at meridian flow. Ask questions about emotions of the associated element. As you are listening to the answer, energetically clear the Yang meridian from the associated organ out the channel. repeat 9 times. Repeat the initial process again and the issue should be resolved.
Thoracolumbar Fascia
The thoracolumbar fascia (TLF) is a large area of connective tissue - roughly diamond-shaped - which comprises the thoracic and lumbar parts of the deep fascia enclosing the intrinsic back muscles.
Most developed in the lumbar region, it consists of multiple layers of crossthatched collagen fibres that cover the back muscles in the lower thoracic and lumbar area before passing through these muscles to attach to the sacrum.
In the thoracic region, it forms a thin covering for the extensor muscles of the vertebral column. Medially, it is attached to the spines of the thoracic vertebrae, and laterally it is attached to the ribs, near their angles. In the lumbar region, it is also attached to the vertebral spines, but in addition it forms a strong aponeurosis that is connected laterally to the flat muscles of the abdominal wall.
Medially, it splits into anterior, middle and posterior layers. The first two layers surround quadratus lumborum and the last two form a sheath for the erector spinae and multifidus muscles. Below, it is attached to the iliolumbar ligament, the iliac crest and the sacroiliac joint. Via its extensive attachment to vertebral spines, the thoracolumbar fascia is attached to the supraspinous and interspinous ligaments and to the capsule of the facet joints.
The unyielding character of the deep fascia enables it to serve as a means of containing and separating groups of muscles into relatively well-defined spaces called ‘compartments’. The deep fascia integrates these compartments and transmits load between them.
The TLF is a critical part of a myofascial girdle that surrounds the lower portion of the torso, playing an important role in the following functions:
load transfer
Stabilization
The connection that the thoracolumbar fascia (TCLF) has with the posterior ligaments of the lumbar spine allows it to assist in supporting the vertebral column when it is flexed by developing fascial tension that helps control the abdominal wall
When the spine is placed in full flexion, the TCLF increases in length from the neutral position by about 30%. The expansion in length of this tissue is accomplished by a tightening in width. This deformation places ‘strain-energy’ into the tissue, which should be recoverable in the form of reduced muscle work when the spine moves back in extension
Load Transfer between Upper and Lower Limbs
Recent studies have highlighted the importance of the thoracolumbar fascia in integrating the activity of muscles traditionally regarded as belonging to the lower limb, upper limb, spine or pelvis and whose action is thus often considered in that territory alone. They have shown that a common attachment to the thoracolumbar fascia means that the latter has an important role in integrating load transfer between different regions.
In particular, these studies have proposed that gluteus maximus and latissimus dorsi (two of the largest muscles of the body) contribute to coordinating the contralateral pendulum-like motions of the upper and lower limbs that characterize running or swimming. They suggest that the muscles do so because of a shared attachment to the posterior layer of the thoracolumbar fascia.
Occipital Fascia
Occipital Fascia attaches to the skull along a continuous line along the superior nuchal line and mastoid processes of the occipital bone. This line of attachment continues anteriorly, just inferior to the boney external auditory meatus, to the zygomatic process of the temporal bone.
Fascia Thickening Affects Balance And Symmetry
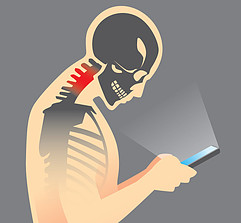
Watch someone while standing or walking down the street while they are texting. See the shoulders rolled forward? The neck is extended out and the head tilted down. If the person is also walking the stride is shortened and erratic. This is then repeated many times per day. While performing this action, the posture is temporarily collapsed. The fascia then thickens at the base of the occipital plate of the scull, the occipital notch. and the origin at the cervical vertebra. How does the thickening of fascia affect balance? In the example above where the person is texting while walking we observe the neck extended and the head looking down. The center of gravity has changed. Our head, on average, weighs 11 to 12 pounds or 4 – 5 kg. The 7 cervical vertebrae in our necks are the support system. If your head is forward and looking down just one inch, about a 15 degree tilt forward, the gravitational strain on these vertebrae more than doubles to about 27 pounds. The person in our example, fully into texting, has a 60 degree tilt and 60 pounds or gravitational strain! That’s 5 times the weight of the head! The fascia’s nerves, the fibroblasts, sense this as a trauma. They thicken all the attachments to compensate for the strain. If this issue happened once in a while, for a short time, the pattern would return to homeostasis, which is the normal healthy balanced state of being. Do it on a daily basis, several times a day and the pattern become entrenched.
This person will have a more difficult time turning the head and standing up straight. Pain will be a constant companion. We haven’t even talked about the shoulders or hips yet. The same process is going on in the shoulders, where there is little structure at all! The shoulder basically just floats with only soft tissue holding it. Rolled forward shoulders has an even more immediate change in pattern than the neck, because of the lack of structure supporting it. Now this person not only has neck problems, but can no longer throw a ball to their dog or child and even placing a dish on the top shelf becomes a major chore! This person now has a balance issue as well, because the head and shoulders are forward, the center of gravity is off and falling becomes a regular issue. Serious injury ahead is a strong probability.
Plantar Fascia

Sole of the foot Deep fascia (planter fascia) Planter aponeurosis
In the past, the plantar fascia has received more attention from the biomechanical engineers and clinicians than from anatomists. This is evident also analyzing the anatomical terminology. In the Nomina Anatomica (1998) only the term plantar aponeurosis is used to indicate this structure, but it is inserted in the chapter ‘fasciae’. In the various anatomical textbooks, the terms ‘plantar fascia’ and ‘plantar aponeurosis’ are used interchangeably. In fact, the term ‘aponeurosis’ is generally used to indicate a tissue with a unidirectional arrangement of collagen fibers, whereas a fascia is a structure with a multidirectional arrangement of the fibers.
No published works have discussed which term is more appropriate for this tissue and it is not clear whether the PF contains only longitudinal or also multidirectional fibers. In our microscopic study, different stains were used to reveal the arrangement and composition of the plantar fascia: the collagen fibers were found arranged mainly in a proximal-to-distal longitudinal direction, but there were also various fibers lying in vertical, transverse and oblique directions.
This multilayer configuration of the collagen fibers is a typical feature of fasciae rather than aponeurosis, so we suggest that the term ‘plantar fascia’ would be a more appropriate name for this tissue. With the imaging stains, it was possible to affirm that almost all the tissue is formed of type I collagen; only in the loose connective tissue where the large fibrous bundles change directions is there also type III collagen. Few elastic fibers could be revealed in the loose connective tissue, but generally we can affirm that the plantar fascia is not an elastic tissue.
The PF was found well innervated, especially where it joins with the fasciae of the abductor hallucis and abductor digiti minimi muscles, and where the sole muscles are inserted. The presence of Pacini and Ruffini corpuscles – usually considered responsible for mechanoreception, suggests that plantar fascia innervations have a role in proprioception and in the stability and control of foot movements.
In the last years there has been increasing interest within therapeutic communities concerning the role that fascia plays in musculoskeletal strain disorders such myofascial pain, postural strain patterns and proprioception but nothing has been published about the possible proprioceptive role of the plantar fascia. However, our findings reinforce previous studies about the antebrachial fascia, the thoracolumbar fascia and ankle retinacula.
Thanks to the many muscle insertions, the plantar fascia is capable of perceiving both the foot's position and the state of contraction of the various intrinsic muscles of the foot. If these muscles contract excessively, the PF (and the nerve endings it contains) might be overstretched. These properties of the plantar fascia shed new light on this complex tissue. The fascia could be seen as a coachman guiding the muscles in the sole of the foot and helping to coordinate all these structures during movement.
The presence of hyaluronan (HA) inside the plantar fascia is an intriguing finding. It enables the different fibrous bundles to glide, as well as being an efficient shock absorber and possibly also serving an anti-inflammatory purpose. Fragmented HA seems to have highly angiogenic, inflammatory effects, and reflects tissue stress. Allowing increased flow of hyaluronan through the manipulation of the tissue could increase the visco-supplementation of the PF, reduce stress and friction between collagen fibers, and contain PF inflammation and degeneration.
The accumulation of tensile stress in the PF is probably responsible for the progressive chondrodysplasia of the calcaneal entheses of the PF, and it could be seen as an adaptive mechanism to ensure the integrity of the interface in response to greater mechanical loads. Our findings thus confirm the gradual shrinking of the anatomical connection between the PF and the Achilles tendon. The relationship between the PF and the Achilles looses connective tissue was also confirmed by our MRI data showing a statistically significant correlation between their thicknesses. Various authors have recently emphasized the role of the loose connective tissue in the etiology of tendinopathy.
In the setting of this study, five of 27 patients with Achilles tendinitis had a PF more than 4.5 mm thick, whereas none of the patients whose MRIs showed no signs of tendinitis had a PF more than 4 mm thick. The thickness of more than 4.5 mm using MR and ultrasound represent fasciitis and in a systemic review it was found that patients with chronic plantar heel pain are likely to have a thickened plantar fascia.
Iliotibial Tract

The iliotibial tract or iliotibial band (also known as the IT band) is a long fibrous reinforcement of the fascia latae. The action of the muscles associated with the IT Band and the tensor fascia latae as well as some fibers of gluteus maximus flex, extend, abduct, and laterally and medially rotate the hip. The IT Band greatly contributes to lateral knee stabilization. This system is only found in humans.
The part of the iliotibial band which lies beneath the tensor fascia latae is prolonged upward to join the lateral part of the capsule of the hip joint. The tensor fasciae latae effectively tightens the iliotibial band around the area of the knee. This allows for bracing of the knee especially in lifting the opposite foot.
The gluteus maximus muscle and the tensor fasciae latae insert into the Iliotibial tract.


Leave a comment
Comment as a guest: